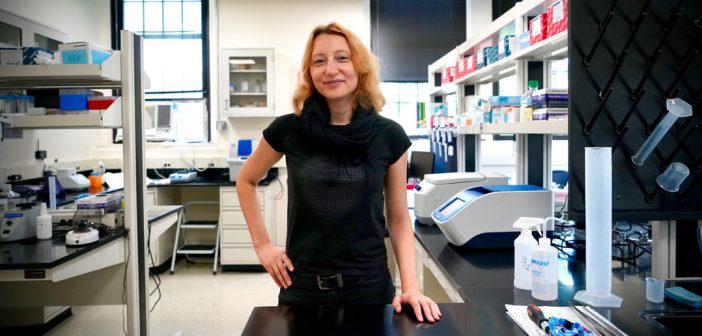
Marija Kundakovic, Ph.D., assistant professor of biology, spearheaded a study that was published in Nature Communications, the third highest-ranked multidisciplinary science journal in the world, earlier this summer. Kundakovic and her colleagues found that chromatin, a microscopic cell component, changes its shape during the ovarian cycle—especially when females experience a drop in estrogen. This changes how our genes behave. Because this occurs inside the brain area implicated in anxiety and depression, it may mediate women’s vulnerability to increased risk for these disorders.
Now, thanks in part to the research conducted by Kundakovic’s team, scientists are closer to figuring out which molecules should be targeted with drug treatments, particularly for women with anxiety or depression.
“This is really important for us to show at the molecular level—the molecular basis of this is what we now, with our study, are starting to understand,” Kundakovic said.
Part of the reason why this study is important is that it focuses on the female brain. Tell me more about that.
The majority of neuroscience experimental studies were done on males. It’s been like that for decades. We know very little about the female brain, and this is particularly a problem for the disorders that are more frequent in women than men, like depression and anxiety. So this is why we basically don’t understand anything about the mechanism that tells us why this sex difference exists.
Our study was designed to try to understand how—at a molecular level—these fluctuating sex hormone levels might increase the risk of anxiety and depression in women.
Why is there such a stark difference between men and women regarding their risk for anxiety and depression?
When you look at boys and girls before puberty, there’s really no difference in risk for depression. This risk really becomes two times higher in females when they get their first period —when the hormones start fluctuating. And then around perimenopause, this difference becomes even more profound because there are more extreme fluctuations. You can have very high or very low sex hormones. And then after menopause, when women achieve these very stable, low sex hormone levels, the sex difference becomes almost nonexistent. So this really tells us that this is not about low or high hormones, but the fluctuations in hormones that might be increasing women’s vulnerability to anxiety and depression.
What’s an extreme example of hormone fluctuations?
Postpartum depression, a period when you have very high progesterone and estrogen (sex hormones), and then a drop after pregnancy. It often triggers a serious depression. There are a lot of lines of evidence showing that this drop in sex hormones, particularly estrogen, may increase the risk for anxiety and depression.
There’s another interesting phenomenon. Women who are depressed and on antidepressant treatments often report that just before their period, they experience worsening of their symptoms. The symptoms seem to be in control with the treatment, but all of a sudden, in this particular period, their symptoms worsen.
All these human findings are consistent with our findings in mice (women experience the menstrual cycle; female mice experience a similar process called the estrous cycle), showing that a drop in estrogen during the estrous cycle leads to increased anxiety levels in females.
You studied brain cells from both female and male mice, and also included female mice in different stages of the estrous cycle. What did you find?
DNA is six-and-a-half feet long in a single cell. You have to package it very nicely so you can put this huge piece of DNA into every cell. The way this is accomplished is through a special structure called chromatin.
This is important to package our DNA, but not only for that. By opening and closing chromatin, you can turn genes on or off. You have to have this open structure for some factors to bind and to turn the genes on. If this is closed, you can’t do that. People use libraries as an analogy. You can have a huge library. There are certain books you can’t even access. But if something’s accessible, you can potentially read it. That’s how our genome works as well.
What we show—and this is really the biggest discovery of this study—is that as hormones fluctuate, they’re actually changing the organization of chromatin. This changes gene expression.
Can you provide an example that explains these chromatin changes?
Serotonin is a neurotransmitter—a chemical in the brain that has been implicated in anxiety and depression. What we show in our study is that the genes that are important for serotonin function, their expression, and their chromatin organization changes with the estrous cycle. Basically, now we are providing a possible molecular mechanism for why we could have those changes in anxiety levels across the ovarian cycle.
What’s the difference between chromatin in male and female mice?
In terms of how many open chromatin regions we have, the numbers are pretty similar. What is different is which regions are open or closed. They change with the estrous cycle, and they differ between males and females, meaning some genes that were closed will open up. And some genes that were open will close. What we didn’t expect is that we would find as many differences across the estrous cycle as we see when we compare chromatin in males and females.
Women and men currently have the same treatment for anxiety and depression. But might your study results lead to the development of sex-specific treatments for these disorders?
Yes. We are starting to understand what are the players involved, what are the mechanistic factors—like receptors, regulators of chromatin—that are leading to this opening and closing. It may help us identify a candidate that we could possibly target with drugs.
Many women take birth control. How can that affect sex hormones and treatment?
We don’t know enough about that. There are different contraceptives. I think we need more studies in humans to understand how exactly contraceptives would affect this.
What implications does this research have for transgender people? Or is there not enough data yet?
That’s another important question that I’m getting more nowadays. What we’re talking about here are biological changes that are induced by hormones. When we talk about transgender people, you might think about certain hormonal treatments that they are receiving. Our brain, even in adulthood, is responsive to these hormones. But sexual differentiation of the brain is very complicated, and it starts very early during life. So as you said, I think we would need more information and funding to try to understand how exactly this would affect transgender people.
This interview has been edited and condensed for clarity.